Imagine that your joints degenerate to the point where you are in constant, severe pain. You are wary of surgery, but your doctor tells you there’s a better method: stem cells. Somehow, he’s able to use stem cells to regenerate your joints or repair your spine. This isn’t something out of science fiction or a vision from a far-flung future: it’s the present. When you have the right stem cell doctor in Santa Monica by your side, you can heal your joints and spine without surgery.
Restoring Your Painful Joints with Your Own Stem Cells
At OrthoRegen, our Gold Standard in Stem Cell Therapy combines four regenerative Orthopedic procedures including two types of stem cells (fat and bone), PRP, and Dextrose Prolotherapy. That’s a lot of reparative cells and growth factors to do the job of healing and repair! Most other regenerative medicine clinics only utilize one or two, at best. By using all four, we’re able to offer our patients a better, more comprehensive treatment. It’s important to realize these cells are autologous. That means they come from your own body, and we’re simply returning them to the injured areas of your body for repair and regeneration.
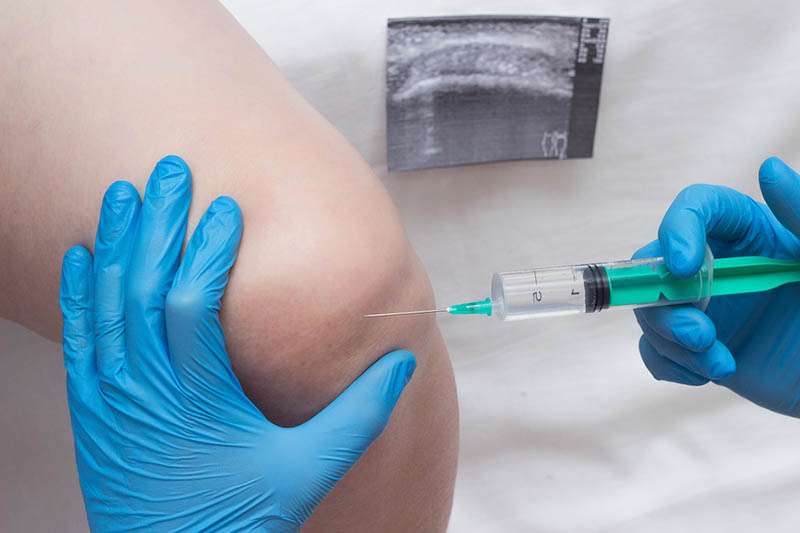
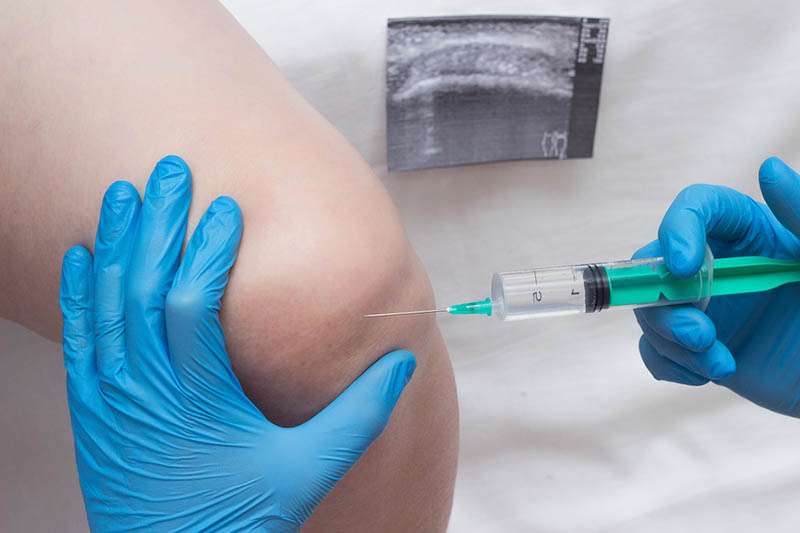
Injecting the Stem Cells
Once we’ve drawn the regenerative cells, we centrifuge them and/or concentrate them. Through this process, we’re able to get a solution that has the highest possible amount of regenerative cells. Then, we inject them right into the injured or degenerated joint. The regenerative cells and growth factors get right to work boosting the healing cascade, so the joint can repair. Stem cells can regenerate all different kinds of joint structures: ligaments, meniscus, cartilage, and bone. So if joint structures are damaged, Regenerative Orthopedics has a great chance of repairing them.
Incorporating Platelet Rich Plasma
We also use Platelet Rich Plasma (PRP) as part of the Gold Standard in Stem Cell Therapy to accelerate the healing. PRP uses plasma derived from your own blood, with a highly concentrated amount of blood platelets. What makes these blood platelets so special is that they can speed up the body’s healing process through their vast amount of growth factors.
Dextrose Prolotherapy for Stabilization
The final Regenerative Orthopedic procedure we utilize is Dextrose Prolotherapy. With Prolotherapy, we inject a dextrose solution to trigger a mild inflammatory response in the body. This is the process the body naturally uses as part of the healing cascade. The tendons and ligaments are generally low in blood supply, and this technique stimulates the blood flow which provides these structures with the nutrition they need for healing. Dextrose Prolotherapy gives the body this boost to get the healing process into high gear. As part of Stem Cell therapy, the Dextrose Prolotherapy to the ligament and tendon structures on the outside of the joint repairs these injured joint structures so the joint can move normally, in a stable and normal fashion.
Contact Dr. Fields, Stem Cell Doctor in Santa Monica
For most patients, only a handful of treatments are required for repair. That’s often far less time (especially considering recovery time) than surgery would require, to say nothing of how much pain surgery could leave you in. Wondering if you’re a good candidate for our stem cell treatment? Schedule an appointment with us by calling 310-453-1234.

Avoid Knee Replacement With Regenerative Orthopedics
Knee pain, like all other types of joint pain, can appear suddenly or become an ongoing, chronic condition. And the most common cause of chronic knee pain and disability is arthritis, which frequently results in knee replacement. In this article, we will discuss ways to avoid knee replacement.
Click to See Stem Cell Testimonial Videos
Knee Pain and Its Common Treatments
Knee pain can be caused by conditions like bursitis, tendonitis, sports injuries, degenerative joint disease, chondromalacia patellae and meniscal injury. All of these very often lead to the eventual surgical recommendation or intervention.
Before surgery, other more conservative therapies are usually attempted to bring relief from the knee pain. NSAIDs (non-steroidal anti-inflammatory drugs like Ibuprofen or Naprosyn) and steroid (cortisone) injections might be included in those initial recommendations.
Are Steroids and NSAIDs Good Choices to Avoid Knee Replacement?
Steroid injections and NSAIDs have been shown in studies to be effective in decreasing inflammation and providing pain relief in the short-term. Unfortunately, they have also been shown to change the properties of ligaments and other soft tissue. And those changes end up slowing down the healing process.
Because these medications inhibit soft tissue healing, their use is cautioned in those who have ligament and soft tissue injuries. Therefore, they should only be utilized for the shortest period of time, if used at all. Since they inhibit healing, they speed up the chance for joint replacement. So, they really are not a great choice if you are looking to avoid knee replacement.
Instead, Regenerative Orthopedic techniques, such as Stem Cell Therapy, PRP and Prolotherapy should be sought, because they have been shown to strengthen and resolve ligament injuries, repair meniscal injuries, and rebuild cartilage in the knee.
The RICE Protocol Is Pretty Common. Is it a Good Way to Avoid Knee Replacement?
So what about the RICE (rest, ice, compression and elevation) protocol? Everyone knows about the RICE protocol. And most people are quick to put it into action. It has to be a good choice. Right? Not really!
An interesting point is that the RICE protocol has been rescinded by its author due to its detrimental effect on healing. What? Yup! The RICE protocol actually hinders blood supply to the injury. And blood brings the healing factors to an injury. Remember…The river does not flow when it is frozen; and that ‘river’ is your blood.
What about Hyaluronic Acid Injections? It’s Natural, Isn’t It? So That Means It Must Be Good!
Hyaluronic acid injections, such as Synvisc or Hyalgen, are some of the most popular conservative treatments for knee pain. Yes, hyaluronic acid is a substance naturally found in the body that provides cushion and lubrication to the joints. And it can be used as an oral supplement and as an injection that is given directly into the knee joint for the relief of knee pain.
But are there drawbacks to the use of hyaluronic acid?
One drawback of hyaluronic acid is that if relief is actually experienced with hyaluronic acid injections, it is generally only for a short period of time. Also, studies have shown this treatment actually lacks clinical effectiveness. In fact, a systematic review of 89 studies that included over twelve thousand patients comparing hyaluronic acid injections to a sham treatment or to no intervention at all, found that hyaluronic acid supplementation to the knee produced minimal to non-existent results when it came to pain relief and function in knee arthritis patients.
That means thousands of patients in these studies received no relief at all. And if they did find relief, it was not much. Unfortunately, those that do find some pain relief with the use of hyaluronic acid, only experience results for a short period of time. And the treatment frequently becomes only a delay for the inevitable knee replacement, because all it does is lubricate a dysfunctional joint, and does not fix anything. In the end, it may delay the joint replacement, but does not help to avoid knee replacement.
Are Cortisone Injections Really All That Bad for the Knee Joint?
Steroids are used to provide anti-inflammatory relief in affected areas of the body. They lessen swelling, redness, itching and allergic reactions. And, in addition to their use for pain, they are also often used as part of the treatment for a number of different diseases, such as severe allergies or skin problems, asthma, or arthritis. In many of these cases, steroids are lifesaving!
The discovery that steroids could be injected into joints was received with enthusiasm, and led to widespread use. However, shortly after doctors started injecting cortisone and other steroids into knee joints in the 1950s, reports of terrible arthropathies, or joint diseases, began to surface. There was an obvious indication that all was not well with this treatment choice. Way back then, the researchers discouraged the use of steroids being injected into the joint, due to their side effects and cell death in the bone.
Steroid injections accelerate cartilage degeneration and joint destruction. Cortisone has a deleterious effect on soft tissue healing by inhibiting blood flow to the injured area, new blood vessel formation, protein synthesis, fibroblast proliferation and ultimately collagen formation.
Cortisone weakens collagen and therefore soft tissue such as ligaments and tendons, which contributes to the development of conditions such as arthritis. And, as we know, this leads to the eventual knee replacement. Today, despite the dangers, cortisone use is widespread and has become the standard of care.
Surgical Repair
Elimination of knee pain by arthroscopic shaving, cutting, or removal of tissue just delays the pain for a few years until the remaining tissue becomes degenerated. The athlete or any knee pain patient must realize that with each procedure and each shaving or cutting of tissue, NSAID prescription, or steroid injection, the risk of developing long-term arthritis and the eventual knee replacement is greatly increased. The key to keeping the knee strong is to stimulate the area to heal. Remember, once surgery is done, it cannot be undone!
Other Non-Surgical Treatments
Even though the goal of many non-surgical treatments such as weight loss, exercise, physiotherapy, bracing, and orthotics, is to decrease pain and improve knee function, they are unable to repair the source of the pain, the ligament or soft tissue injury. Why is it so important to repair the ligaments and other soft tissue? Because the long-term consequence of ligament and soft tissue injuries that are left unhealed is arthritis.
Is it any wonder the treatments mentioned above, including hyaluronic acid, do not last. And why they are unable to prevent the eventual knee replacement! You see, these treatments are unable to get to the root cause of the problem. The road to arthritis can only be remedied when the problem of ligament injury is addressed. None of the above treatments address this problem. But Regenerative Orthopedics does.
Regenerative Orthopedics Is An Effective Treatment to Avoid Knee Replacement
Regenerative Orthopedic therapies such as Stem Cell Therapy, PRP and Prolotherapy stimulate, rather than interfere with, the normal healing process. The treatments stimulate the normal inflammatory-reparative mechanisms of the body, boosting cartilage growth, strengthening the tendons and ligaments, and repairing the meniscus in a knee or the labrum in the hip or shoulder.
These regenerative treatments offer hope to those suffering from various types of knee pain and provide an effective, non-surgical option for those trying to avoid knee replacement.
As we say at OrthoRegen®:
Regenerate First; Surgery Last!